As the skiing and snowboarding season approaches, Advanced Orthopedic Specialists will be seeing many patients who unfortunately have sustained an injury during their vacation. Our team of sports medicine specialists is prepared to care for any injury that can occur while on the slopes. Below we will discuss some of the more common injuries sustained while skiing or snowboarding.
Simple Precautions to Follow
For starters, it is very important that all skiers or snowboarders wear a helmet. This is the biggest safety measure available to protect the head. It is also very important that you stay well hydrated as you travel to higher altitudes so you can perform at your best and enjoy your time as much as possible. Anybody who has sustained altitude sickness knows this can ruin an excellent vacation.
When hitting the slopes, it is important that the individual knows his or her limits and does not try to tackle runs that are outside of their ability. This is one of the more common causes of injuries.
Finally, the snowboarder/skier should never partake in any alcohol consumption prior to skiing, which impairs your judgement.
COMMON Skiing INJURIES
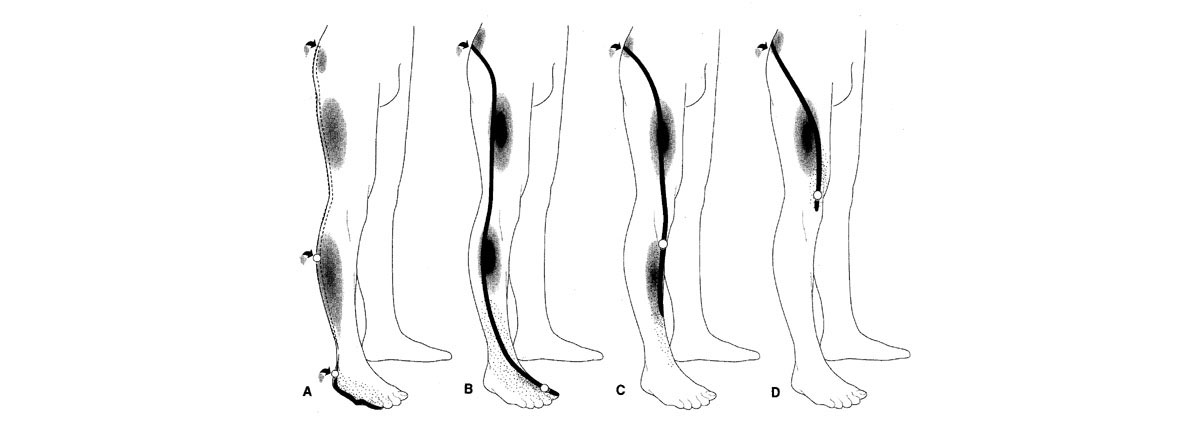
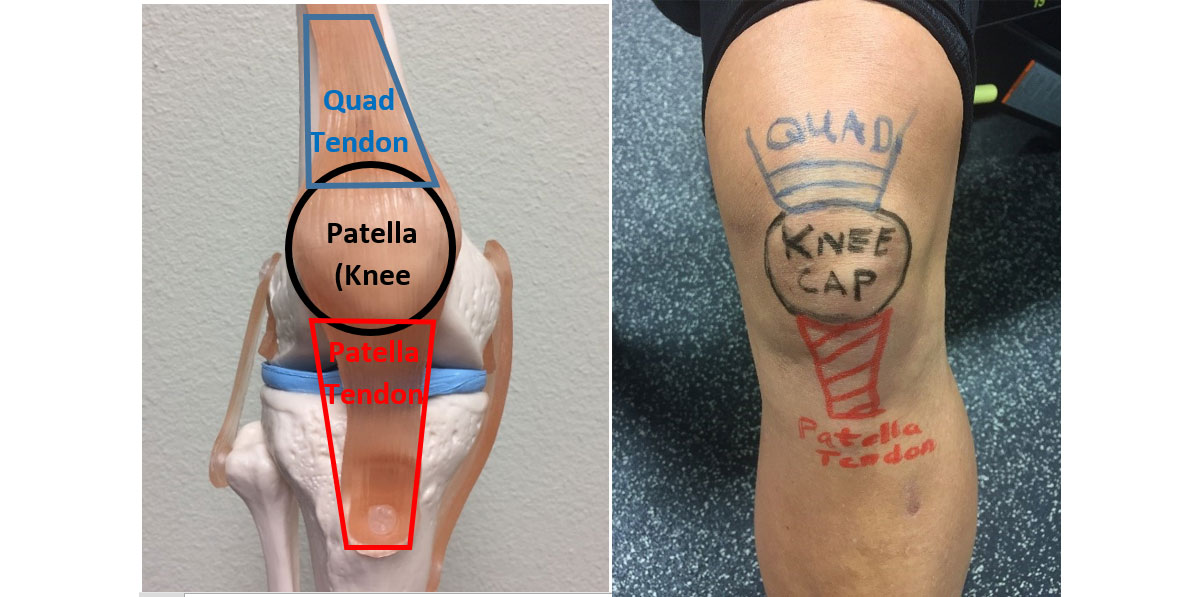
Skiing injuries most commonly affect the lower extremities. In fact, the knee is the most common joint injured while skiing. Knee injuries can include a tear of the anterior cruciate ligament or the meniscus, which are usually treated operatively. Other common knee injuries are the medial collateral ligament, which is treated nonoperatively, or the tibial plateau. The tibial plateau is the top of the tibia. It is not uncommon with any torquing injury to sustain a tibial plateau fracture, most of which are treated with limited weight-bearing. However, some can be displaced and require surgical fixation.
Typically, knee injuries in skiers are sustained when the ski twists, the bindings do not release, and there is significant torque placed upon the knee. This torque typically causes injury to the medial collateral ligament (or the ligament on the inside of the knee) and if the force continues, it can tear the anterior cruciate ligament and/or fracture the tibial plateau.
If you sustain an injury where the bindings do not release, you feel a pop and have severe knee pain, you should not attempt to ski down the hill, but rather call ski patrol, and be transported to the bottom of the hill where you can be evaluated by a specialist. The majority of ski resorts now have orthopedic surgeons or emergency physicians available at the base where they can treat your injury temporarily until you are able to get home for further evaluation.
Tibial fractures can also occur. This, unfortunately, is sustained with a very high torque to the tibia and can cause a fracture. This commonly is treated with surgical fixation onsite at the ski resort.
One common injury that often goes unnoticed is an injury to the thumb. This can happen when a direct force is applied to the tip of the thumb while the wrist is going in the opposite direction and tears the ligament at the base of the thumb. This is actually called “skiers thumb.” The technical term is a tear of the ulnar collateral ligament. The skier may experience difficulty grasping. This needs to be evaluated when you return home.
Common Snowboarding Injuries
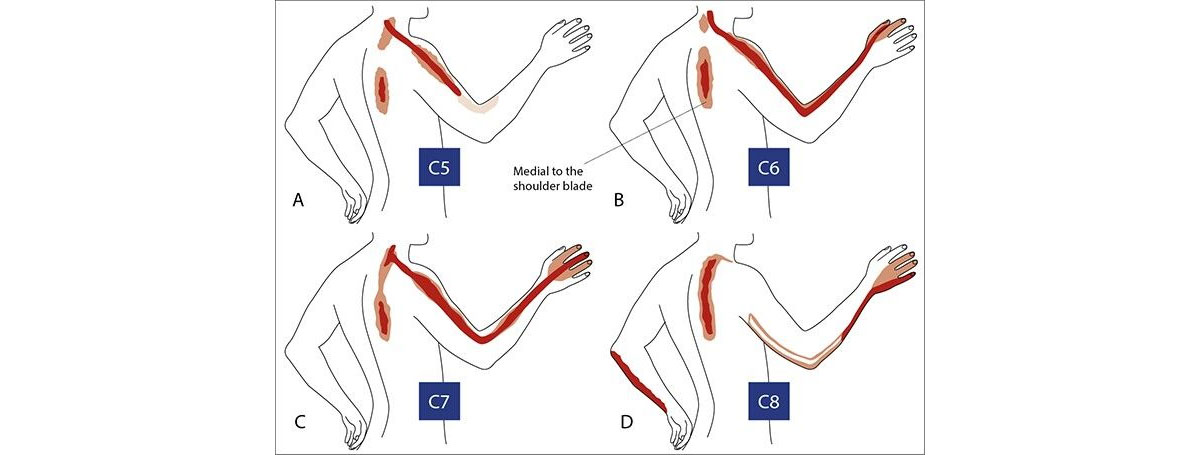
Snowboarding has become more popular in recent years. The majority of snowboard injuries involve the upper extremity. We commonly see injuries to the clavicle, most of which can be treated nonoperatively. Also an injury to the acromioclavicular joint, which is toward the tip of the shoulder. This occurs with a fall directly onto the shoulder and these are treated nonoperatively. It is recommended that the snowboarder obtain an x-ray, be placed into a sling, and then follow up with the orthopedic surgeon upon their return home.
Snowboarders also commonly fall onto the outstretched arm and can sustain injuries to the elbow, such as elbow sprains and possibly a fracture. If you sustain a significant fall on the outstretched arm and have severe elbow pain, you should obtain a radiograph and then be placed into a splint and follow up with the orthopedic surgeon.
Finally, the snowboarders can experience injuries to their hands and wrist, such as wrist sprains and/or wrist fractures. Again, this should be evaluated by the local clinic with x-rays, splinting and follow up with an orthopedic surgeon upon returning home.
Helping You Get Back to the Slopes
All the physicians of Advanced Orthopedic Specialists are avid skiers. We also see a tremendous amount of skiing injuries during the winter and do our best to treat you without surgery and get you back to feeling better as soon as possible. However, if surgery is necessary, we would help get you back on the slopes once your injury resolves.
If you’ve sustained an injury or need a second opinion, schedule an appointment with us now!