With fall just around the corner, it’s also time to start thinking about falls. As an interesting fact, September 23rd is the first official day of fall in the Northern Hemisphere, as well as Fall Prevention Awareness Day. For adults 65 years or older, falls are the leading cause of fatal and non-fatal injuries leading to broken hips, wrist fractures, head injuries and decreased quality of life. Indirectly, falls and fear of falling can lead to decreased social engagement, declining independence, and poor mobility thereby affecting mental health and contributing to feelings of helplessness.
A Look at the Statistics
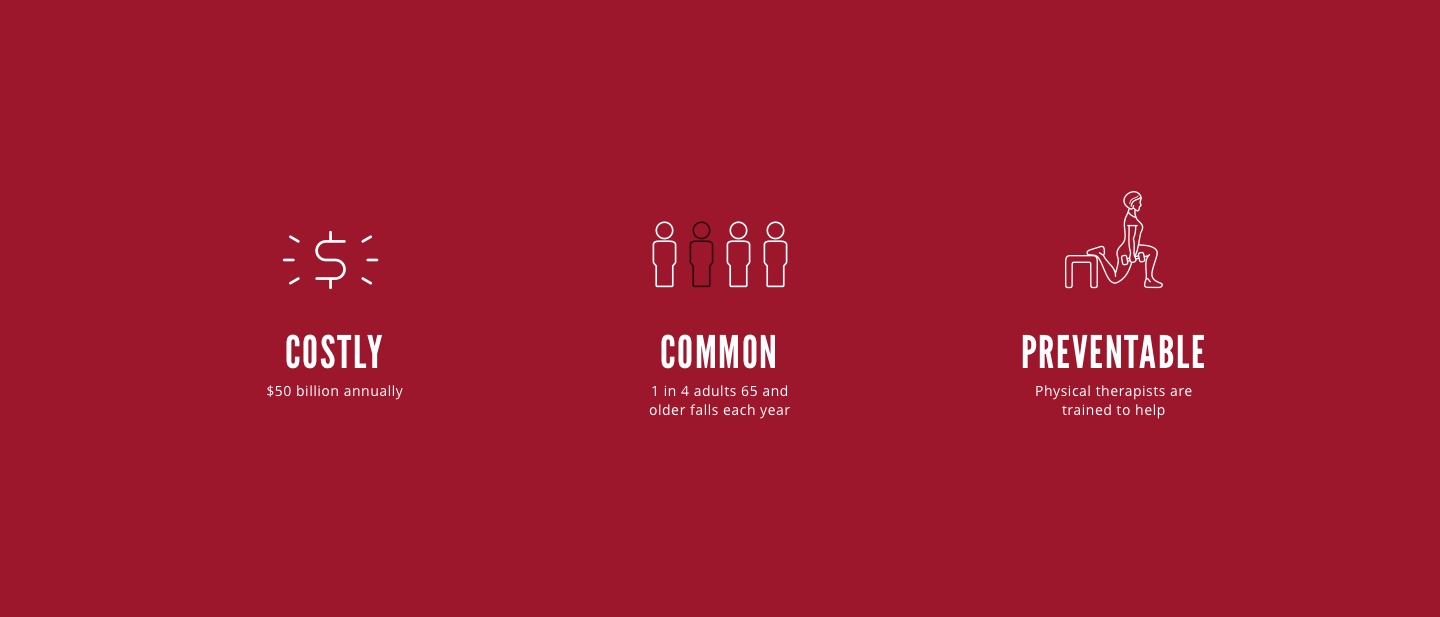
Annually, 1 in 4 older adults will experience a fall resulting in approximately $50 billion dollars spent treating the aftermath. Most of these costs are hospital-related with over 800,000 older adults being admitted annually at a rate of 1 every 11 seconds with fatalities resulting once every 19 minutes. The financial cost of these traumas, approximately 75%, falls on Medicare and Medicaid. If falls rates are not reduced, direct treatment costs are projected to reach $101 billion by 2030.
Risk Factors to Consider
Falling is not a normal part of aging, but as people get older a multitude of factors contribute to injuries or death as a result of a fall. Below are risk factors. The more you have, the greater the risk of falling.
- History of falls
- Being female
- Sedentary lifestyle
- Overall poor health
- Recent hospitalization
- Advanced age
- Poor balance, due medical condition, such as stroke, Parkinson’s Disease, Multiple Sclerosis, diabetes
- Leg weakness
- Easily fatigued
- Limited flexibility
- Problems with vision or touch sensation (diabetic retinopathy or peripheral neuropathy)
- Getting dizzy when you stand up from sitting or lying down (orthostatic hypotension)
- Trouble with memory and thinking
- Joint pain/arthritis
- Taking too many medications or taking certain types of medications
- Depression and/or anxiety
- Home hazards, such as throw rugs, poor lighting, or a lack of handrails on stairs
- Inappropriate footwear
- Inappropriate use of a walker or a cane
Can a Physical Therapist Help?
Yes! Many risk factors for falls are modifiable, and physical therapists are specifically trained to recognize and address complicating factors that directly and indirectly contribute to falls. Even during routine evaluations, unrelated to falls, a physical therapist may ask older adults about their fall history. I always tell my patients it’s much easier to address balance than to recover from a hip surgery.
How Does a Physical Therapist Assess and Treat Balance and Falls?
First, we gather your current and previous history. A physical therapist will start with questions regarding fall history, activity level, medications, sensations of dizziness, faintness when changing position or feelings of fatigue with ambulation. In addition to physical symptoms, your physical therapist will address your environment, such as footwear, assistance at home, and home layout. We look to you to help identify what contributing factors you’re already experiencing.
Once we have your history, we move onto your physical presentation. For this portion we exam lower body strength, flexibility, sensation of the feet (specifically for diabetics), and vision. Most importantly, we assess your balance through formal and informal testing. During a formal balance assessment, a physical therapist will utilize a test, such as the Berg or Tinetti to generate a score. This score is taken upon initial evaluation and periodically retested to assess your improvement as well as determine the level of fall risk. Informal testing consists of gait analysis, observation of transfers, and lower body structure.
Following the initial evaluation, your physical therapist will recommend what you can safely begin at home. We will develop a formal plan of care specific to your needs that will be carried out in the clinic. In addition, you will also receive a home exercise program as well as recommendations to make your home environment safer and easier to navigate.
Six Exercises to Help Prevent Falls
These exercises help prevent falls by challenging your balance in a safe manner. If you’re unable to perform these exercises then you may want to have your balance formally assessed.
- Standing March: Stand in place and start marching in place slowly for 20-30 seconds. As this becomes easier, challenge your balance and change up the surface you are marching on: from hardwood to carpet, foam pad, grass, etc.
- Standing 3-Way Kicks: Standing on 1 leg (with a soft knee, not locked in full extension), move the other leg in front of you (keeping your leg as straight as possible), then out to the side, and then behind your body. Perform 10 times on each side.
- Sidestepping: Walking alongside (facing) a countertop or near a wall (with hands on the surface as needed), step sideways in 1 direction with your toes pointed straight ahead. Move 10 steps in 1 direction, then return in the other direction. As this becomes easier, use a resistance band just above the ankles.
- 1-Leg Stand: Stand on 1 leg as long as you are able, up to 30 seconds. Alternate legs, and try to do this 3-5 times on each leg. As this becomes easier, challenge yourself by doing other tasks while standing on 1 leg, such as brushing your teeth, talking on the phone, or while doing biceps curls.
- Sit to Stand: Rise out of a chair without using your arms to push up. If this is difficult at first, use a firm pad underneath you (to place on chair seat) to raise you as you need. Perform 10 times.
- Tandem standing or tandem walking: Place 1 foot directly in front of the other, so the heel of the front foot touches the toe of the back foot. Maintain standing in this position as long as you are able, or up to 30 seconds. As this becomes easier, try taking a few steps in this heel-to-toe format, as if you are walking on a tightrope. Remember to use something to hold on to for safety.
With falls being a significant cause of morbidity for older adults, there is an abundance of resources for patients, family members, caregivers, and healthcare professionals. Listed below are various resources based on the Stop Elderly Accidents, Death & Injuries (STEADI) Initiative from the Centers for Disease Control and Prevention (CDC) and the University of North Carolina.
Resources For Patients
STEADI Initiative / Postural Hypotension
Stay Independent Brochure
What You Can Do to Prevent Falls
RESOURCES For Caregivers/Family Members
STEADI Initiative / Protecting Loved Ones
Check for Safety
RESOURCES For Healthcare Professionals
STEADI Initiative / Evaluation Guide for Older Adult Clinical Fall Prevention Programs
Source Material
Falls Prevention Awareness Day 2018 Impact Report. (2018).
Mulcahy, J. A., PT, MPT. (n.d.). 6 Balance Exercises You Can Safely Perform at Home.
Shubart, T., PT, PhD. (2011, June 2). Physical Therapist’s Guide to Falls.